Recurrent Malaria: Understanding the Cycle of a Persistent Threat
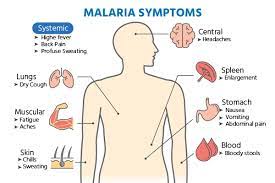
Malaria, a mosquito-borne infectious disease caused by the Plasmodium parasite, continues to be a major global health concern especially in Africa. While significant progress has been made in reducing malaria-related deaths and cases over the past few decades, one particularly challenging aspect of this disease is recurrent malaria. Recurrent malaria refers to the reappearance of symptomatic malaria infections in an individual after an initial infection has been treated and resolved. This phenomenon can have serious health and economic implications, making it imperative to better understand its causes, risk factors, and prevention measures.

Malaria
Recurrent malaria, also known as relapsing or recurrent infections, occurs when the parasite persists in the body and causes multiple symptomatic episodes of the disease. This article explores the various aspects of the treatment of recurrent malaria, including the causes, diagnosis, and evolving treatment strategies.
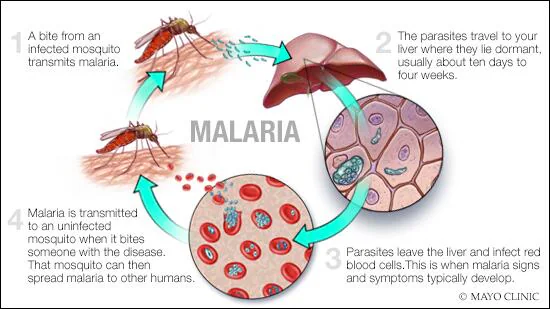
The Lifecycle of Malaria
To comprehend recurrent malaria, it’s essential to understand the life cycle of the malaria parasite, which primarily involves two hosts: humans and female Anopheles mosquitoes.
- Mosquito Bite: The cycle begins when a female Anopheles mosquito infected with the Plasmodium parasite bites a human to feed. During this blood meal, the mosquito injects sporozoites, the infectious form of the parasite, into the human’s bloodstream.
- Liver Stage: Once inside the human body, the sporozoites travel to the liver, where they infect hepatocytes and replicate extensively. This asymptomatic stage of infection can persist for days or even weeks.
- Blood Stage: After maturing in the liver, the parasites are released into the bloodstream as merozoites, where they infect red blood cells (RBCs). This stage is responsible for the clinical symptoms of malaria, including fever, chills, and anemia.
- Transmission: When an infected mosquito bites another human, it ingests gametocytes, the sexual forms of the parasite, during the blood meal. Inside the mosquito, these gametocytes mature into sporozoites, completing the cycle.
Recurrent Malaria: Causes and Mechanisms
- Dormant Liver Stage: In some cases, after an initial infection is treated and resolved, a few parasites may remain dormant in the liver. These parasites can reactivate weeks, months, or even years later, leading to recurrent malaria. This is particularly common in the case of Plasmodium vivax and Plasmodium ovale infections.
- Incomplete Treatment: Poor adherence to antimalarial medications or the use of ineffective drugs can lead to incomplete clearance of the parasites from the bloodstream. This leaves room for the parasites to multiply and cause a relapse.
- Antigenic Variation: Plasmodium falciparum, the most deadly malaria parasite, has the ability to change the surface proteins on infected RBCs. This antigenic variation allows the parasite to evade the host’s immune system, making it difficult to develop lasting immunity.
- Drug Resistance: The emergence of drug-resistant strains of the parasite, particularly P. falciparum, poses a significant challenge in treating and preventing recurrent malaria. Resistance to commonly used antimalarial drugs like chloroquine and artemisinin derivatives has been reported in various regions.
Understanding Recurrent Malaria
Recurrent malaria primarily occurs due to two main reasons:
- Reinfection: Individuals living in malaria-endemic regions are at risk of being repeatedly infected with the parasite through mosquito bites. This reinfection can lead to recurrent episodes of malaria. Preventing reinfection often involves strategies such as the use of insecticide-treated bed nets and indoor residual spraying to reduce mosquito breeding and bites.
- Relapse: Some Plasmodium species, such as P. vivax and P. ovale, have a unique ability to form dormant liver stages known as hypnozoites. These hypnozoites can reactivate weeks, months, or even years after the initial infection, causing recurrent malaria. This phenomenon is particularly common with P. vivax infections.
Diagnosis of Recurrent Malaria
Accurate diagnosis is crucial for effective treatment of recurrent malaria. Diagnostic methods include:
- Microscopic Examination: Microscopic examination of blood smears remains a gold standard for diagnosing malaria. It allows for the identification of the Plasmodium species causing the infection and can help distinguish between relapse and reinfection.
- Rapid Diagnostic Tests (RDTs): RDTs are useful in settings with limited access to microscopy. They detect specific malaria antigens in a blood sample, providing rapid results.
- Molecular Testing: Polymerase chain reaction (PCR) assays can detect low levels of parasites and identify the species accurately. PCR is particularly valuable in research and epidemiological studies.
Treatment Strategies for Recurrent Malaria
The treatment of recurrent malaria depends on several factors, including the Plasmodium species involved, the patient’s age and health status, and the region’s drug resistance patterns. Here are some key aspects of treatment:
- Antimalarial Drugs: Antimalarial medications are the cornerstone of recurrent malaria treatment. Commonly used drugs include:
- Artemisinin-based Combination Therapies (ACTs): ACTs are recommended for the treatment of uncomplicated malaria and are highly effective against P. falciparum, the most deadly species. Examples include artemether-lumefantrine and artesunate-amodiaquine.
- Chloroquine: Chloroquine is effective against P. vivax and P. ovale, which can form hypnozoites. It’s often used to treat relapses of these species.
- Primaquine: Primaquine is crucial for the radical cure of P. vivax and P. ovale infections. It targets the hypnozoite stage in the liver.
- Tafenoquine: Tafenoquine is another drug used to prevent P. vivax relapses, particularly for individuals unable to tolerate primaquine.
- Drug Resistance: Resistance to antimalarial drugs, particularly P. falciparum resistance to artemisinins, is a growing concern. Combating resistance involves using combination therapies and continuous monitoring of drug efficacy.
- Preventive Measures: In areas with a high risk of recurrent malaria, preventive strategies such as intermittent preventive treatment (IPT) and chemoprophylaxis are recommended.
- Vector Control: Reducing mosquito exposure through the use of insecticide-treated bed nets and indoor residual spraying can help prevent reinfection.
- Community Engagement: Community-based interventions and education about malaria prevention, early diagnosis, and treatment-seeking behavior are crucial in reducing the burden of recurrent malaria.
Conclusion
The treatment of recurrent malaria is a multifaceted challenge that requires a combination of effective drugs, diagnostic tools, and preventive measures. While progress has been made in recent years, ongoing research and surveillance are essential to address emerging drug resistance and ensure that individuals living in malaria-endemic regions receive timely and appropriate treatment. Additionally, efforts to develop new drugs and vaccines continue to hold promise in the fight against recurrent malaria, with the ultimate goal of eliminating this devastating disease worldwide.